Rosenthal Receives NIH Grant to Develop Non-Addictive Pain Treatment, Addressing Opioid Crisis

Opioids are widely used pain treatments, despite their relative ineffectiveness for chronic pain and their high potential for misuse and addiction. There is an urgent need for alternative, non-addictive pain treatments.
The National Institutes of Health (NIH) recently awarded a grant to MBL Senior Scientist Joshua Rosenthal to further his research on blocking pain signals through site-directed RNA editing, a technology he is developing for biomedical applications following fundamental research with squid.
The grant is through the NIH’s Helping to End Addiction Long-Term (HEAL) Initiative, dedicated to funding science-based solutions to the national opioid public health crisis. Rosenthal’s five-year, cooperative-agreement grant seeks to end with a lead candidate for clinical drug trials.
Among the non-addictive pain treatments currently approved by the FDA are drugs that block the transmission of pain signals -- specifically, by blocking voltage-gated sodium ion channels (Nav) in the nervous system. These drugs can sometimes provide symptomatic relief for patients but have worrisome side effects affecting the brain and heart. They are also difficult to generate and are rapidly cleared from the body, limiting their effectiveness.
Rosenthal and his colleagues on the grant propose a novel approach to modifying Nav channels that doesn’t rely on small-molecule blockers. Studies of human pain disorders and animal models of pain have validated Nav1.7, which is preferentially expressed in peripheral neurons (outside of the brain) as an attractive target for therapy. Rosenthal’s team proposes to use site-directed RNA editing to render the Nav1.7 channel permeable to both sodium and potassium, creating a counter-current that will dampen the neuron’s excitability (and pain signal) more effectively than blocking the channels. This work underscores the vast therapeutic potential of RNA editing-based strategies for altering molecular properties rather than blocking molecular function.
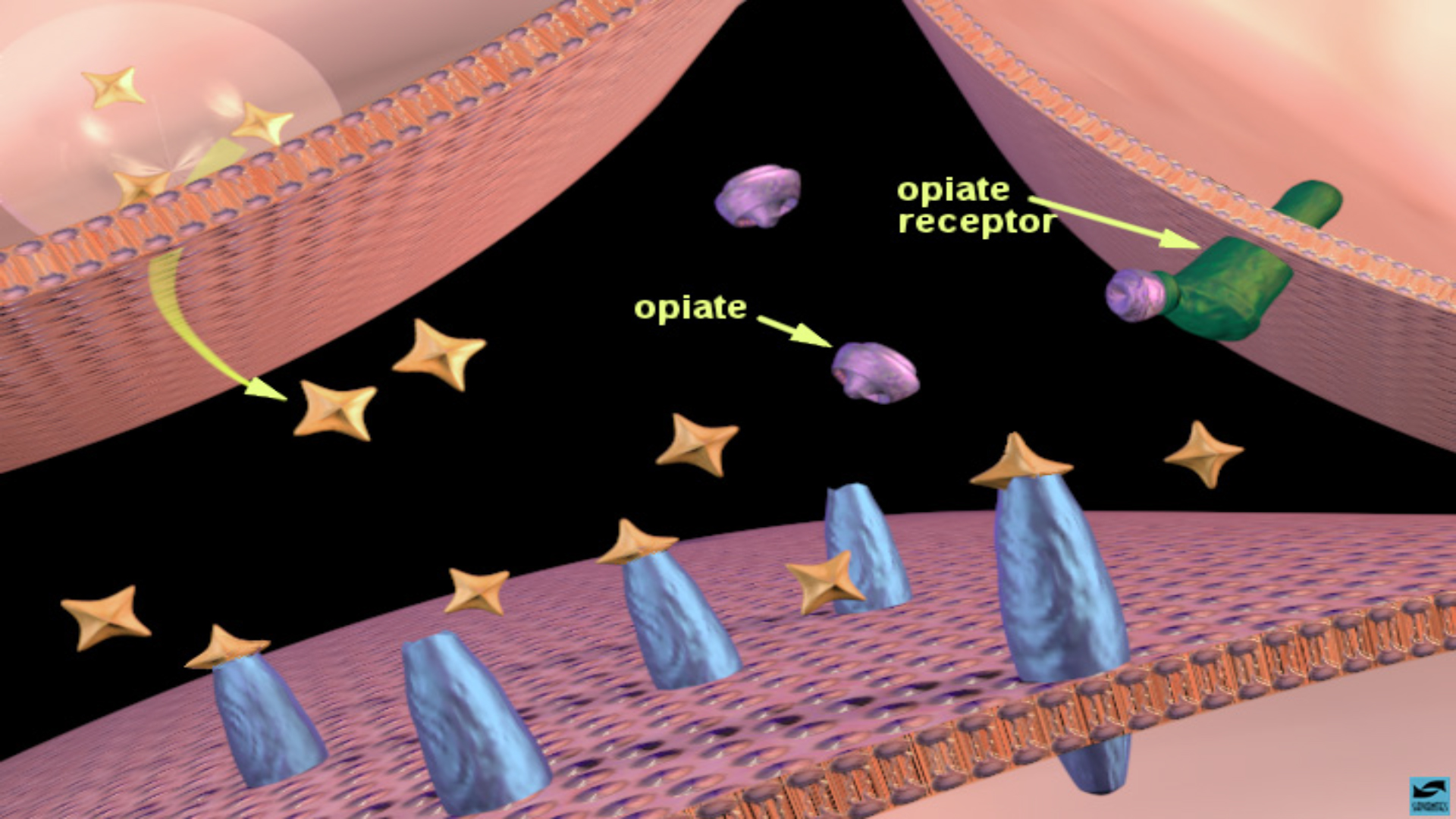 Opioids include legal, prescription pain relievers, the illegal drug heroin, and synthetic opioids such as fentanyl. When opioids enter the brain, they bind to receptors both in the “pain pathway,” leading to pain relief, and in the “reward pathway,” creating a feeling of euphoria or “high” via the release of dopamine. Regular use can lead to dependence, addiction, overdose and possibly death. In this illustration, opiates bind to opioid receptors in the nucleus accumbens, leading to increased dopamine release.
Opioids include legal, prescription pain relievers, the illegal drug heroin, and synthetic opioids such as fentanyl. When opioids enter the brain, they bind to receptors both in the “pain pathway,” leading to pain relief, and in the “reward pathway,” creating a feeling of euphoria or “high” via the release of dopamine. Regular use can lead to dependence, addiction, overdose and possibly death. In this illustration, opiates bind to opioid receptors in the nucleus accumbens, leading to increased dopamine release.Credit: National Institute on Drug Abuse
Rosenthal’s collaborators on the grant are Gregory Dussor of University of Texas-Dallas, Sulayman Dib-Hajj of Yale School of Medicine, and Eli Eisenberg of Tel Aviv University.
“More than 47,000 Americans died of opioid overdose in 2017,1 and more than 2 million Americans live with addiction to opioids. Moreover, more than 50 million Americans suffer from chronic pain, and of those, 25 million live with daily chronic pain2 and lack effective and safe non-opioid options for pain management,” according to the HEAL Initiative’s website.
“The widespread use of opioids to treat acute and chronic pain contributed to the approximately 10.3 million people aged 12 years and older in the United States in 2018 who misused opioids, including heroin.4 These staggering numbers are likely underestimates.”
Rosenthal’s award comes through the National Institute of Neurological Disorders and Stroke.